“Prevention is better than cure,” the Dutch philosopher Desiderius Erasmus once observed.
Clearly, Erasmus’ maxim – first mentioned in the 1500s – had staying power: the phrase is now ubiquitous in healthcare circles and healthy-lifestyle campaigns.
Application of the “prevention principle,” however, has been the real challenge. Nowhere is this more evident than in the area of drug diversion.
Missing Drugs
Recent studies bear this out: the US and Canada – two countries struggling with “unprecedented opioid-related mortality” rates – have “unexplained losses” of controlled substances which are demonstrably high.
This begs the question: how do you prevent what is unexplained?
An examination of healthcare systems also reveals a concerning disjunction: though one will find protocols for the handling of controlled substances – such as Fentanyl and Oxycodone – in most hospitals, comprehensive prevention safeguards to prevent diversion are frequently absent.
Without these safeguards in place, it’s far easier to divert controlled substances and foster serious harm than you might imagine – especially when you know the system.
Samantha’s Story
The truth is, few know the system like nurses. Though diversion can happen at any point along the supply chain, nurses with the easiest access are most likely to misuse prescription drugs, with the highest rates of abuse among nurse anesthetists.
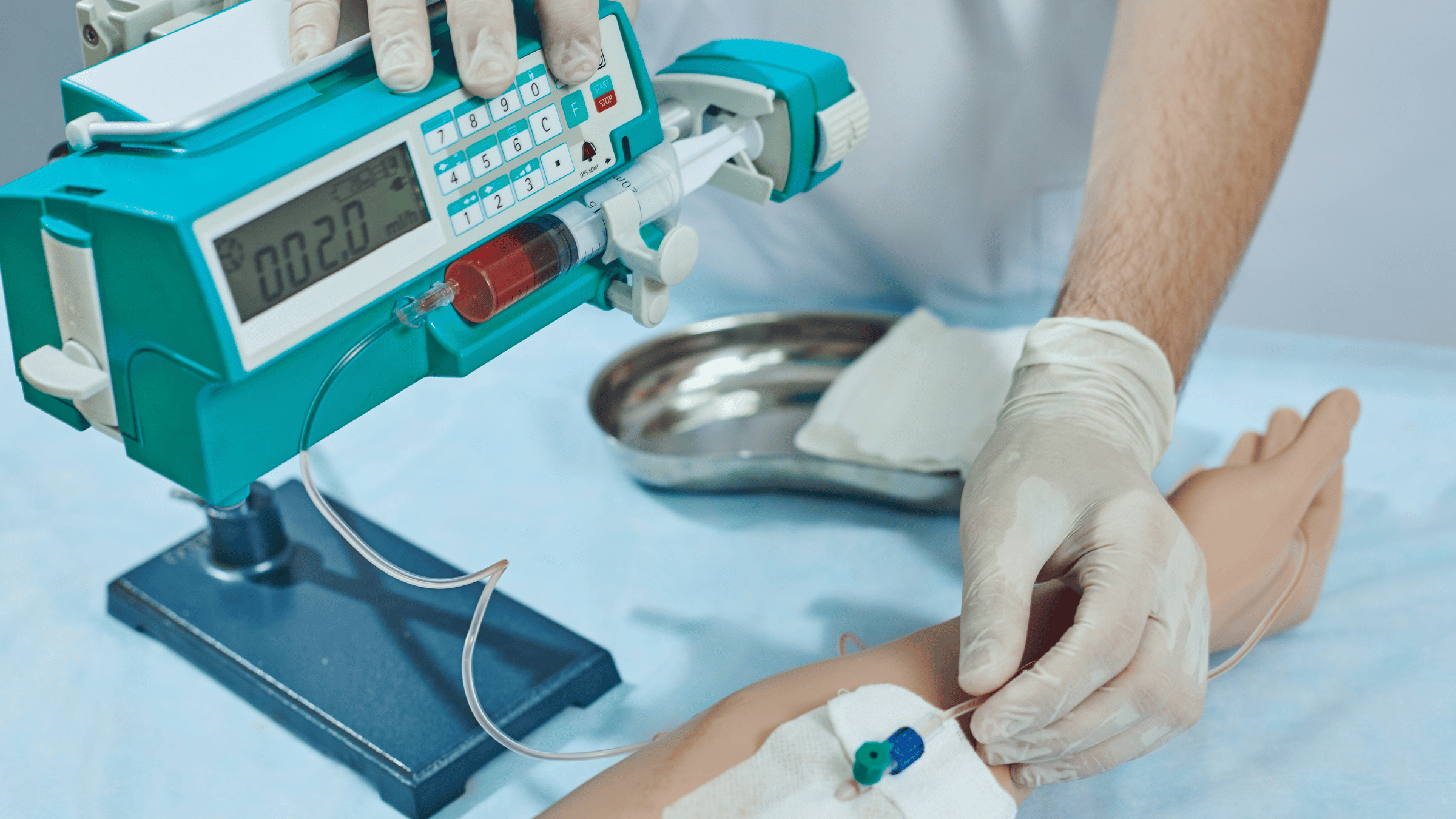
Reasons for this include access (they are the primary administers of controlled substances), and a powerful mix of stressors: frequent bouts of grief, frayed emotions, and physical exhaustion. Often, the temptation to divert will be right in their lap – literally.
This was Samantha’s* story. As she tells it,
“As I was changing out of my scrubs after returning home from my shift, I realized there was a leftover amount of IV pain medication in my pocket.”
We can imagine the moment: holding the needle up to the light, enticed by the potent liquid within. How would it feel? Has to be better than I’m feeling now, she must have reasoned.
Samantha placed the needle into her medicine cabinet, where it stayed for a week.
It’s true what they say about access, how it opens the door to opportunity. Curiosity can also entice us, fooling us into believing our motives are harmless, even justified.
So when the desire for comfort was strongest, Samantha found an insulin needle and injected herself with the medication. The results were immediate:
“As the medication hit my bloodstream, I literally fell to my knees and felt like all the pain in my life was draining out of me. And that was it. That was enough for me to start down the path of ruining my career.”
Cheating the System
“Hospitals have come up with a multitude of protocols to avoid the abuse of controlled substances,” Samantha notes, “but they are extremely easy to get around.”
For example, most hospitals utilize fingerprint scanning and required codes to retrieve medication from a Pyxis machine. When medication is drawn up and/or excess is wasted, it’s protocol that a second nurse be present to witness and sign off.
“However, it’s widely known that nurses are understaffed, and very rarely do they have time to stand by and watch this protocol completion from start to finish,” Samantha says.
Another means to cheat the system is to give less of a dose than what was ordered. “For instance, 1 mg of morphine may be ordered for the patient, but an addicted medical professional can easily give them half the dose, saving the remainder for themselves.”
Perhaps it’s not surprising then that one study revealed that nearly 8% of controlled substance medication transactions showed discrepancies between the medication dispensed and the medication administered.
Of these discrepancies (amounting to 4 million in the study), 9% of cases were reviewed but were marked as “unable to be reconciled” – clearly suspicious for diversion.
45% of those cases were not reviewed by hospital officials. That’s 1.8 million cases left open and unresolved.
“The primary reason is usually a lack of time, combined with a lack of priority,” Douglas J. Zurawski, Pharm.D., says. “This priority needs to be set at the senior executive level to provide the level of urgency around variances. It really does come from the top down, and across all departments in the hospital.”
The Risks are High
Hospitals must find a way to counter this, for as the research reveals, drug diversion has tangible impacts and far-reaching implications – all with human faces attached:
- Patients, who “suffer insufficient analgesia or anesthesia, experience substandard care from impaired Healthcare Workers, and are at risk of infections from compromised syringes.”
- Healthcare workers are not only “at risk of overdose and death; they also face regulatory censure, criminal prosecution, and civil malpractice suits.”
- Hospitals, who “bear the cost of diverted drugs, internal investigations, and follow-up care for affected patients, and can be fined in excess of $4 million dollars for inadequate safeguards.”
- Negative publicity and losing public trust are unfortunate but very real outcomes as well.
- The public, as “diverted drugs impact population health by contributing to drug misuse.”
Protocols aren’t Safeguards
What are the measures that must be prioritized, then, to enable prevention and save lives?
First, there must be a serious acknowledgment that protocols alone aren’t enough.
Standards alone are insufficient. Accepting that effective safeguards are also needed to prevent possible drug diversions before they occur is a critical first step.
For instance, the research mentioned above regarding the US and Canada’s “unexplained losses” of drugs highlights the problem – yet we know that protocols exist. Why then, for example, could a US endoscopy clinic not account for $10,000 of missing propofol in just one four-week period? How could this not be traced?
The report implies that acknowledgment, while vital, is insufficient unless it leads to action: “A lack of traceability [a necessary safeguard] is needed to understand the root causes of the loss.”
As the research concludes, “Hospitals require guidance to assess their drug processes against known vulnerabilities and identify safeguards that may improve their capacity to prevent or detect diversion.”
Second, guidance must provide a holistic approach to diversion and mitigation safeguards. This is the work of proven drug diversion specialists.
Drug diversion prevention requires a multi-faceted, holistic approach, combining people, processes, and technologies.
System-based strategies will require “careful configuration of healthcare technologies and processes in the hospital environment [which] can reduce the opportunity for diversion.”
Rxpert Solutions understands the value of such an approach, providing:
- Staff surveys and leadership interviews to assess current attitudes, behaviors, policies, and procedures related to the handling of controlled substances.
- Expert policy and procedure evaluation, inventory management evaluation, diversion prevention program analysis, and provide recommendations for improvements.
- On-site diversion prevention risk assessment to identify risks of diversion and ways to mitigate those risks.
- Evaluations of the current investigation and reporting process as well as recommendations for improvement.
- Current staff and leadership education programs toward the goal of incorporating everything from the prevalence of diversion to recognizing the signs of substance abuse in their peers and reporting requirements.
- Centralized diversion monitoring via access to the facility’s software surveillance data.
Importantly, hospital administrators and front-line staff must provide active participation and support of such measures.
Third, assessment of current technologies for possible gaps is invaluable.
For example, traceability must involve a system of safeguards that provide layers of safety and identification.
This may include the use of:
- Strategically-placed cameras in vulnerable areas
- Biometric (eg, fingerprint) signatures
- Computerized verification of transactions (in case a live witness is not present)
- Rapid removal of discharged patients to prevent additional dispensing of drugs
- Additional technologies
Without such safeguards, substances will continue to be diverted.
Prevention Starts Now
Wise guidance is needed to meet the growing problem of drug diversion. Holistic care will move beyond acknowledgment and protocols to tangible actions and effective safeguards.
Rxpert Solutions exists to provide this guidance. Our proven assessments combine skilled, experienced personnel with effective drug diversion prevention and mitigation technologies to provide a systemic solution – because we can all agree: prevention is, indeed, better than cure.
* Not her real name